Find a Doctor
We've got you covered with access to over 1 million doctors, hospitals, and health facilities. Search by name or provider type in our online provider directory.
Search For Care
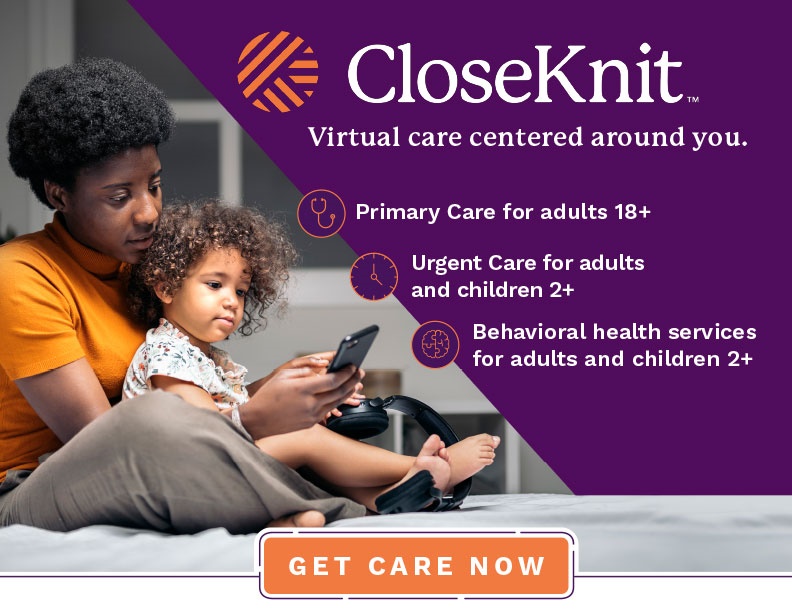
A new patient-centric, virtual-first primary care practice. Compassionate care for over 100 conditions through an easy-to-use app. 24/7/365. CloseKnit's care teams offer preventative and urgent care, behavioral and mental health, chronic condition prevention, medication management, and more.
Get StartedCheck out your wellness programs personalized assessments and challenges and members-only discounts on Blue365.
Need care now? We have multiple options to ensure you get compassionate care when and where you need it.
Use our findhelp tool to search for free or low-cost resources in your area anonymously. Find food, housing, transportation, legal services and more.
Programs for Your Health
Achieve total wellness - of mind and body - with CareFirst's support programs. These programs empower you to live your healthiest, for yourself and the people that count on you.
Prescription Drug Tools
View covered drugs, tips to save on prescriptions, participating pharmacies, and more.
Manage Healthcare Costs
You have a right to know what you're paying and why. Explore tools to estimate and compare costs. Plus, spending account resources that offer flexibility.